Hierarchy of Protection Mechanisms – FASCIA/DURA – dysfunctions

FASCIA/DURA Normalization Techniques©
Andrew T. Still, DO said the body will protect different tissues in a Hierarchy of Importance.
1. Vascular, Lymphatics, and FASCIA (in this order)*
2. Nervous System
3. Organs
4. Endocrine System
5. Musculo-skeletal System
* – Vascular, lymphatics, and fascia are integrated, but begin with vascular
FACTS OF FASCIA – Myofascial Meridians
“Anatomy Trains” by Thomas W. Myers
Anatomy Trains provides a “longitudinal anatomy” of twelve individual sets of maps with tracks, stations, and switches. It is a systemic point of view offered as a supplement to the standard analysis of muscular action.
OVERVIEW OF FASCIA
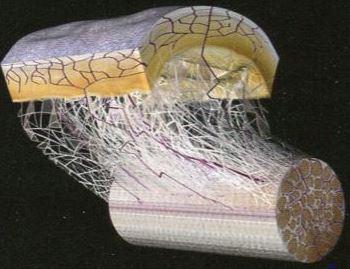
Fascia is a dense meshwork of irregular connective tissue that covers all of our tissues in our bodies. It is around our muscles, organs, joints, brain ligaments, capsules, tendons, vascular and lymph vessels, and nerves (epineurium). (Schleip 2003).
Fascia is the largest sensory system in the body, with a rich vascular and nerve supply present in the outer layers of deep fascia. In the deeper layers we find intra-fascial nerve fibers where the institial myofascial tissue receptors are located (Stecco, et al 2008). They are sensitive to stretch, thermal, and chemical stimuli.
FASCIAL “stretch” REFLEX
Fascia is a common factor in many systems, such as the outer layer of blood vessels, lymph vessels (adventitia) and nodes, and the epineurium (50%) of the nerves all have Type III and IV receptors. These nerve endings run in parallel with the sympahtetic nerves. When they are stimulated, they connect with sympathetic neurons in the grey horn of the spinal cord, and then in turn, connect via efferent fibers to the respective vessel or nerve. These are spinal reflex arches, and they cause constriction of the vessels (smooth muscles in tunica media) and nodes. Constriction of the epineurium causes a reduction in the fascial glide and thereby influences musculoskeletal mechanics (Schleib R, et al) such as joint glide and slide.
Fascia follows the body’s connective tissue forming traceable ‘meridians’. The word ‘meridian’ is usually used in the context of the energetic lines of transmission in the domain of acupuncture. The myofascial meridian lines are not acupuncture meridians, but lines of pull, based on standard Western anatomy; that is, lines that transmit strain and movement through the body’s myofasical around the skeleton. They have some overlap with the meridians of acupuncture, but the two are not equivalent.
The plantar surface of the foot is often a source of trouble that communicates up through the rest of the line on myofascial tracks and bony stations to the head. With this in mind, Patricia M. Kortekaas, PT, found reflex points that would aid in the communication of a fascial line and named them “breakers”. She continued to identify more “breakers” on other points on the feet and hands.
Breakers can be used to restore and normalize the innervation of dysfunctional fascial lines.
The advanced HNT© students learn to address the connection between the fascial lines on a macroscopic level and the joint capsules/ligamentous structures on a microscopic level. They scan for fascial tension along the myofascial track by drawing in at the “breaker”.
A fascial “trauma” is a sudden unexpected pull, compression or shearing force, or a chronic slow impact on a fascial line that will result in a fascial line contraction and neurological dysfunction. Simply, the fascial line has lost its capability to glide and slide at the appropriate time.

FASCIAL BIOMECHANICS© by Patricia M. Kortekaas, PT
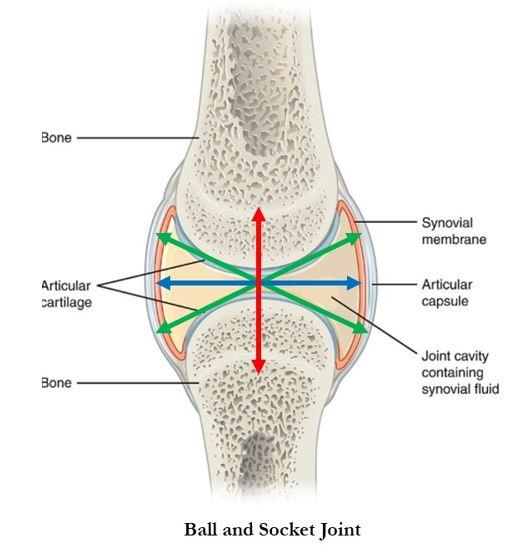
The fibers from the joint casules and ligaments support the glide and slide mechanisms in the joints and need to follow the gross movements from the fascial lines to a well-integrated movement pattern. Patricia realized that every movement is a combination of micro and macro fascia connections in the whole body, even up the the fascia of the organs and the connection with the fascia surrounding the vascular and lymphatic systems. She calls it Fascial Biomechanics©.
Our fascia can be considered our “mechanical brain”. Every neurological input from the brain must innervate the big fascial lines as well as the joint capsules that simultaneously support the smooth and well-coordinated movement patterns in the body. So, it is safe to say that each joint capsule most likely has a combination of connecting fibers to the spiral, the ventral/dorsal and lateral lines, depending on the osteopathic form/shape of the individual joint.
References
Myers, T. W. Anatomy Trains, 2nd edition, Churchill Livingston, 2009, 295 pp.
Schleip, R., JBMT, Jan 2003 “Fascial Plasticity: A new Neurobiological Explanation
Stecco et al, 2008. “The expansions of the pectoral girdle muscles onto the brachial fascia: morphological aspects and spatial disposition“. Cells Tissues Organs. 188:320-9.