Hierarchy of Protection Mechanisms – VASCULAR – injuries
VASCULAR Normalization Techniques©
Andrew T. Still, DO said the body will protect different tissues in a Hierarchy of Importance. We begin with VASCULAR.
1. VASCULAR, Lymphatics, and Fascia
2. Nervous System
3. Organs
4. Endocrine System
5. Musculo-skeletal System
When an injury occurs to the body, there will be a three dimensional impact to the surrounding tissues, especially the impact to neurological, lymphatic and vascular supply of the intra and extra-articular tissues of that area. Protection of these structures is the high priority of the protection hierarchy, and these systems are the most altered in an injury.
When an injury occurs to the body, there will be a three dimensional impact to the surrounding tissues, especially the impact to neurological, lymphatic and vascular supply of the intra and extra-articular tissues of that area. Protection of these structures is the high priority of the protection hierarchy, and these systems are the most altered in an injury.
Because of these alterations, you will see joint or soft tissue restrictions in that area because of loss of glide/slide mechanics in the damaged tissues. This disturbrance of tissues and rhythms arise from the epicenter of impact of the injury. The effect of the impact will steadily diminish in the surrounding tissues in three dimensions, like the ripples caused by a rock thrown in the water.

As a result, there will be a three-dimensional vascular and/or lymphatic stagnation or hemostasis that develops in the affected arteries, capillaries, veins and/or lymph vessels. The fluid, or pressure dynamics in that area will be altered, and tension on the surrounding tissues will build up. The rhythms of the involved tissues will be altered as well, and the body will start to compensate for the altered pressures and restricted flow of fluids. The alterations can appear in the cerebral spinal, lymphatic, vascular, and other interstitial fluids of the body.
The greatest vascular stagnation will be in the venous flow. (There are two times more veins than arterial vessels in the body.) If there is stagnation of venous flow, there will also be an indirect reduction of the arterial flow in that area. As a consequence, tissue healing and regeneration will be impeded.
BLOOD VESSEL PHYSIOLOGY
The heart is a very important mechanical motor, but it is not built to be the master regulator of blood vessels. The sympathetic part of the autonomic nervous system is responsible for the neuro-physiological input to the blood vessels. These reflexes might be related to the vascular mechanics of the walking cycle (gait cycle) in the body.
In our bodies, we see a dynamic interplay of fluid pressures that are regulated by the Central and Autonomic Nervous Systems (CNS and ANS). There are cerebral spinal, interstitial, lymphatic, vascular and intra/extra articular fluids regulated by the ANS. If there is a stagnation of venous blood flow before the diaphragm (e.g., more blood volume below the diaphragm), blood pressure can build up and restrict the venous blood flow from the arms and neck/head region (fluid dynamics).
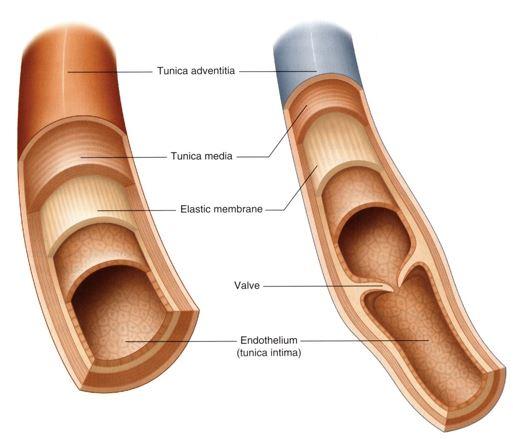
The arterial and venous walls have an inner, middle, and outer elastic membrane (tunica). One of the functions of the elastic tissue is to absorb and store the vascular energy created by the moving blood. Proprioception and protection against stretching forces are other major functions of the elastic membranes. Arteries and veins are innervated by the sympathics of the ANS and receive both motor and sensory innervations.
TRAUMA
Blood vessels are especialy sensitive to quick stretching, shearing or compression forces, and can respond to a vaso-constrictive mode of the elastic membranes of the inner and outer tunicas. These hyperactive reflex responses of the tunicas can create stagnation in the blood flow of the surrounding tissue (i.e., hemostasis).
When there is a strain or sprain of a joint capsule, a “mechanical” joint restriction develops with reduced glide/slide mechanisms. This restriction might be based on restriction of the vascular flow, but the lymphatic flow and/or myofascial dysruption of the capsules and ligaments can not be ignored. Vascular, lymphatics, and the unifying fascia are the three highest levels of protecion hierarchy of the body.
VASCULAR Normalization Techniques (VaNT)©
When we began to recognize these fascial and mechanical restrictions were the result of neurovascular dysfunctions in the joint capsular tissues and fascial planes, instead of true mechanical dysfunctions, we needed different techniques to restore function. For example, restoring the normal mechanical function of a joint means restoring the normal vascular flow and resting level of the nervous system activity to the blood vessels of the affected joint. These specific manipulation techniques of the vascular and nervous system are called Vascular Normalization Techniques (VaNT)©. VaNT© techniques rely on specific reflexes that we have empirically identified. These reflexes are located in certain bones in the tarsal joint (influencing vascular congestion/dysfunction below the diaphragm, including the abdomen, pelvis, and legs); the carpal joint (influencing vascular congestion/dysfunction above the diaphragm, in the chest, arms, and neck). We have found in our clinical practice that using these reflexes help to restore the normal movements of the tissues, normalize blood flow, and in general, encourage restoration of normal physiological function, allowing healing to occur!